One of the most dangerous and frustrating things that can happen is when a pregnancy is found outside the uterus. Ectopic Pregnancy represents 6-14% of all emergency department visits of women with first trimester bleeding. The good news is that that the mortality has decreased significantly since 1980.
The reasons for this may be because we have more sensitive pregnancy tests and better ultrasound equipment. The move to laparoscopic approaches and the advent of medical treatment has also had a role.
The Catholic Church and the Ethical Directive for Catholic Health care have an interesting dilemma.Directive 44 contains the words “Every procedure whose sole immediate effect is the termination of pregnancy before viability is an abortion, which, in its moral context, includes the interval between conception and implantation of the embryo.”
This has led to a spirited discussion about the options: Expectant management (waiting), Salpingectomy (removing a part of or the whole affected fallopian tube). Salpingostomy (remove the pregnancy from the tube) and Medical treatment with Methotrexate.
It is the last two options, which seek to preserve the fallopian tube, which have come under the most scrutiny. Indeed, the Bio-ethicist William May changed his own argument between Edition 1 and Edition 2 of Catholic Bioethics and the Gift of Life.
There was a relatively spirited written conversation between
REV. TADEUSZ PACHOLCZYK, Ph.D. and REV. William GroganWhen Pregnancy Goes Awry – The National Catholic Bioethics Center.
Catholic New World – Applying double-effect principle in ectopic pregnancy.
But the discussion is well developed in an Article in the National Catholic Bioethics Quarterly. In it, the author develops out the full ethical argument and a little of the biology.
But there should be a couple of comments on some of the options
Expectant management. This is a relatively uncommon option used in few options. One is patient driven…the patient feels fine and is willing to see where things go
The other is medically driven. Most doctors who will consider this option will warily watch when the pregnancy test (beta hCG) is 200IU and falling.Some will watch at hCG levels as high as 1000 and falling. One Study (2004) showed that among 107 women with documented ectopic pregnancies, 70% resolved with expectant management. in women with hCG < 175, 96% resolved,but only 21% resolved in women with hCG > 1500. Most importantly, we do not know what level of hCG is critical for tubal rupture, so the higher the initial hormone level, the more careful.
In cases where salpingectomy (removal) of the tube takes place, there is no surefire way to guarantee the health of the other tube. The incidence of recurrent ectopic pregnancy is 15% (range from 4-28%) One review suggested that the risk was lower after salpingectomy (removal) vs salpingostomy (removal of the ectopic and preserving the tube) (9.9%vs 14.8%). The tubal patency (the tube remains open) is very high for salpingostomy and Methotrexate (70-90%)
There have really only been a couple of case reports regarding the transfer of ectopic pregnancies from the tube to the uterus. It is an area worth studying, but it needs a willing participant both in the OR and the MD. Most doctors would not think twice about the needs to extend the medical sciences to try. Of course, early attempts at IVF involved flushing the embryo from one uterus and transferring it to another. And with the advances of IVF labs and the equipment they have, the ability to extract and transfer an embryo is truly possible. The biggest challenge is that the trophoblast of the ectopic tends to invade the tube, so it is very difficult to remove the pregnancy without disrupting it. But it is a real possibility.
As for the definitive Methotrexate teaching……it likely doesn’t exist. But there are a few non-negotiables. The presence of a heart beat should be an absolute contraindication, as should a rising bHCG. However, persistent hCG levels immediately following a salpingectomy or with evidence that the baby has died (falling hCG) then a discussion can be had.
I am sorry to be so technical, but ectopic pregnancy is a subject that is discussed widely. It is another thing, though, that would become much less prevalent if we could reduce the number of couples having pre-marital sex, cohabitating and using birth control. We could probably cut the ectopic prevalence significantly just by welcoming back the culture of life
St Gianna, pray for us!
CUF.org :: Catholics United for the Faith.
Related articles
- Smoking Increases The Risk Of Ectopic Pregnancy (medicalnewstoday.com)
- Future reproductive outcomes for women who have had an ectopic pregnancy (eurekalert.org)
- Future Reproductive Outcomes For Women Who Have Had An Ectopic Pregnancy (medicalnewstoday.com)
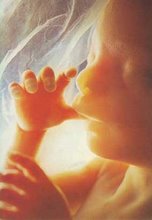
An ectopic pregnancy as seen on ultrasound
Drawing of an ectopic pregnancy from the 17th century by Reinier de Graaf,
copied from an earlier French publication by Benoit Vassal